Psoriasis is a chronic, recurrent, inflammatory skin disease, largely various in morphology, distribution and manifestations, prevalent in a broad range of age and as common as 2% in some populations. According to Henseler, psoriasis may present in two distinguished types, type I and type II. Type I is manifested early in life, first appears in childhood in more than 30% of cases, with a family predisposition and a more severe disease.
Psoriasis association with human leukocyte antigen, HLA-cw6 has been established while its genetic basis appear to be complex, multifaceted and still developing. Seven major loci of susceptibility has been found with 6p21, PSORS1, locus as the main over-represented in all cohorts tested.
Multitude of environmental conditions may stoke the initial disease and bolster its chronicity. Among them, mechanical stress, radiation, UVB, skin irritations (koebner’s phenomenon), drugs, most notoriously, beta blockers, interferons and lithium, vaccination, streptococcal infections, alcohol and smoking may be named. Clinically, the disease is projected with well-circumscribed squamous papules and plaques with silvery scales, dispensed symmetrically on large joints and scalp, in its more prevalent form.
Metabolic syndrome is two times more common in psoriatic patients, that translates into association of coronary artery disease, hypertension, diabetes type II, hyperlipidemia, and increased body mass index with psoriasis. Sustained inflammation which results in hyperkeratosis is the mainstay of its pathogenesis. Neovascularized acanthosis with inflammatory infiltrates including dendritic cells, macrophages and neutrophils characterizes the histology of psoriatic plaques.
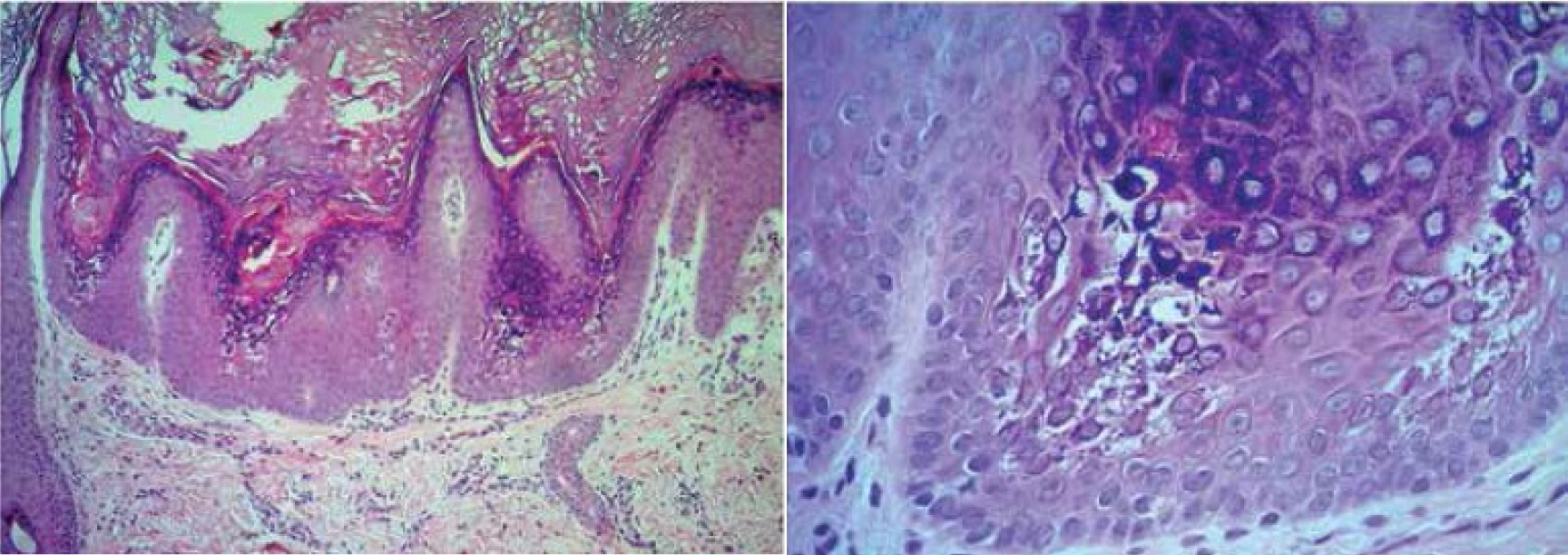
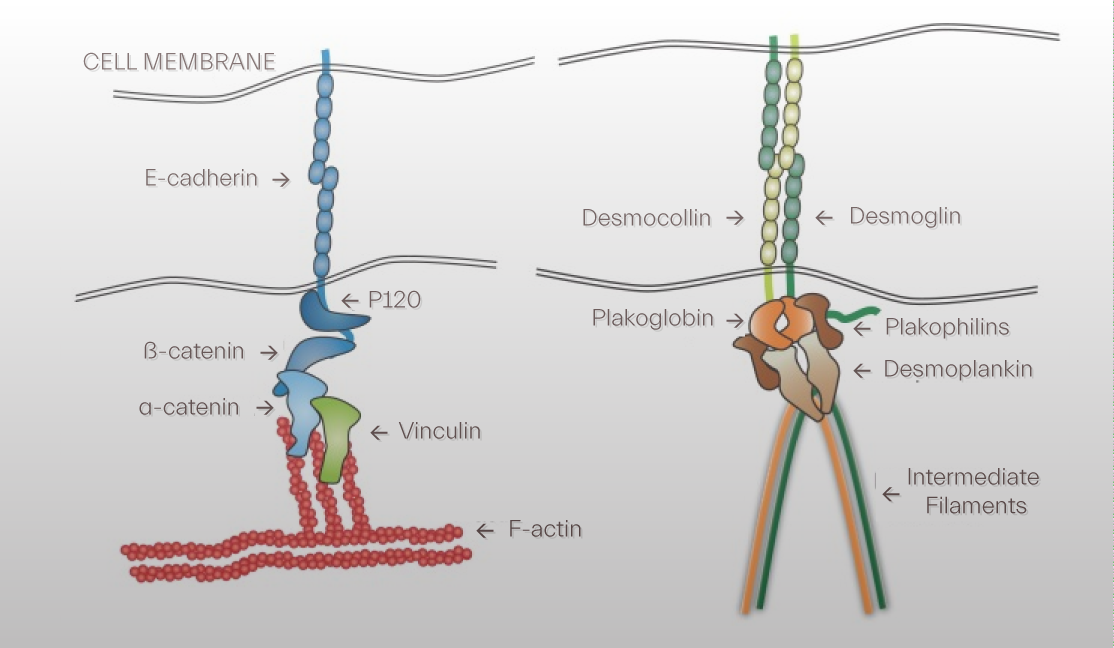
Intercellular junctions, tight, reduced expression, gap, upregulation of conexin 26, and adherens, reduced expression of E-cadherins, junction proteins are found to be disrupted with activation of IL-17, the most notable cytokine in pathogenesis of the disease. Decline in expression of tight junction may be due to transepidermal water loss and is of crucial note in psoriasis topical treatment design.
Cadhereins sense and respond to mechanical signals within and without cells to adjust actomyosin interactions, a process by which they provide strength to adherens junctions while desomosomes couple intercellular connections to intermediate filaments.
Severity of the disease is the centerpiece of therapeutic agenda for psoriasis as mild to moderates disease are treated with topical treatments while more severe cases may warrant a systemic strategy. Psoriasis topical treatment may implicate glucocorticoids, vitamin D derivatives and phototherapy to manage mild to moderate disease. Biolgoics, methoteraxate and retinoids are most notable and widely exercised in treatment armamentarium of severe disease.
Among topical treatment of psoriasis vitamin D derivatives, corticosteroids and keratolytics such as azelaic acid and salicylic acid could be named. They appear less effective yet most safe and convenient to use. Keratolytics support physical skin barrier in the epidermis, spurring differentiation and modulating proliferation as opposed to steroids which enhance the immune skin barrier within the dermis and epidermis and vitamin D derivative which prominently affect the two barriers.
Psoriatic plaques have proclivity for drier skin areas with less sebaceous profusion where dysbiosis appear with leverage and dynamism. These subordinated vicinities of sebum manifest higher biodiversity and less quantity in microbiome. Addressing dysbiosis in a topical formulation seems to be a plausible approach to treatment.
Shingosine, a byproduct of ceramides once cleaved by ceramidase, can be phosphated by a protein kinase. Sphingosine-1 phosphaste have been reported to restrain keratinocytes proliferation and shore up their differentiation and downsize inflammation by curbing dendritic cells migration to lymph nodes. Sphingosine-1-phosphate has been suggested as psoriasis topical treatment by its own or through therapeutics which induces its impact such as 1-25-(OH)2-D3.
Emolients and moisturizers may be used in adjunctive topical psoriasis treatment as they prevent transepidermal water loss and reduce scaling and pruritus while moderating keratinocyte proliferation. Cream and lotion preparations can be formulated with nutrients with anti inflammatory properties not equally effective as steroid creams but less harmful in cutaneous atrophy which may prove their long terms more contentious in a chronic disease.