There is evidence of association between sebum linoleate concentration and comedo formation. Essential fatty acids deficiency contributes to sebaceous gland hypertrophy and hyperkeratinization of the ducts. Linolenic acid level in the stratum corneum has been reported to be much higher in normal subjects than that in the comedones in particular linoleate content of wax esters. Oily cutaneous and hypersecretion of sebaceous glands is well known as one of four major players in pathogenesis of acne [1] [3]. However, change in composition of the secreted oils during acne has been less studied. Studies by Stewart ME, et al suggest that skin’s fatty acid composition may change with changes in sebaceous gland activity, and that sebum fatty acids can enter the epidermis and be incorporated into epidermal lipids [4]. In this article we are going to examine how different composition of oily secretions in acne patients is from those of normal subjects. We have attempted to look across multiple studies reported in dermatology literature to determine if correction of skin surface lipids can control sebaceous gland overactivity which, in turn, may improve acne.
Studies by Downing et al indicates that differrentiating sebaceous cells implement sebaleic acid instead of linoleic acid in wax esters if the later fatty acid is not available [5]. Sebum fatty acid composition is not fixed but changes in relation to sebum secretion rates. Specifically, with increasing sebum secretion, changes appear to occur both in the lipid class composition (more wax esters compared with cholestrol esters [6] and in the fatty acid composition of the ester lipids [7].
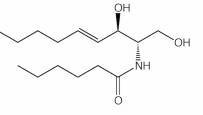
Ceramides, typical structure
Lower amount of sphingolipids and ceramides in keratinocytes of acne subjects of various level of oil level in the skin has been shown [9]. This would be associated in decrease in ability of keratinocytes’ walls to hold water, one possible mechanism that can explain how hyperkeratinization starts in comdeones since impaired water barrier function is concurrently seen in hyperkeratosis. In addition ceramides can trigger nuclear factor-kappa B (NF-kB), leading to induction of human beta defensin-2 (hBD-2) expression, enhancing the skin’s innate antibacterial defense [10].
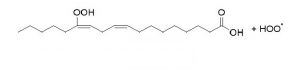
Linoleic acid molecular structure
Although lipogenesis and inflammation are induced by certain propionobactrium acnes strains, sebaceous glands also express proinflammatory cytokines and produce free fatty acids in the absence of bacteria [14]. This may explain a role independent from that of p.acnes for sebaceous gland hyperactivity in pathogenesis of combination skin in acne vulgaris. The same authors [14] suggest generation of antimicrobial peptides by p.acnes in absence of inflammation and proinflammatory cytokines. On the other hand, diets rich in docosahexaenoic acid/eicosapentaenoic acid (DHA/EPA) and gamma-linolenic acid (GLA) have been shown to incorporates metabolites of these fatty acids to epidermal phospholipids, which, in turn, leads to inhibition of leukotriens at the skin level [15].

Alpha and gamma linolenic acid follow two pathways in stark distintion
Increase in plasma androgen level induced by steroids cause an increase in cholesterol and free fatty acids in skin surface. Some essential fatty acids such as gamma linolenic acid are potent 5-alpha-reductase inhibitors, suggesting a linkage between unsaturated fatty acids and androgen action [20]. In adult skin androgen action is dependent to conversion of testosterone to five-alpha-dihydrotestosterone. This conversion takes place under enzymatic act of five-alpha-reductase. Cultured sebocytes strongly express 5-alpha-reducatase and 5-alpha-DHT [21]. Hypersensitivity of androgen receptors in pilosebaceous duct and the resulting increase in sebum production and oily skin appears to be associated with a significant increase in free fatty acids rather than other surface skin lipids, a fact that can be incorporated in development of skincare for oily skin.
High skin’s lipid production and the resulting low level of linoleic acid leads to hyperkeratosis, impaired epidermal barrier function and comedo formation. Stimulation of sebocyte proliferation by insulin, thyroid-stimulating hormone and hydrocortisone indicates that the hormonal control of the sebaceous gland is a complex mechanism [21]. Can providing the skin with essential linoleates prevent comedo formation and aid excessively-oil-forming skin to manage itself? A study reports that stratum corneum sphingolipids of adult acne patients is lower than that in control subjects. Decrease in sphingolipids content of cell walls contributes to diminished water barrier function which, in turn, leads to increased permeability to inflammatory substances and comedo formation . All these studies support use of unsaturated fatty acids in treatment of oily skin in acne vulgaris and call for a campaign against long-been-supported and conventionally-recommended oil-free products for oily skin and acne patients by physicians.
Our hypothetical idea is that hypersensitive overworked sebaceous glands in an acne patient do not operate to produce their high-end products such as linoleates, rather, their overflow is associated with cheap secretions from less-differentiated sebocytes such as free fatty acids. There is an inverse relationship between secretion rates and the linoleate content of the surface wax esters. The question that whether local supply of essential fatty acids down regulate the overworked sebaceous glands is supported by studies of Letawe C, et al. Topical application of linoleic acid resulted in significant decrease in size of follicular casts and microcomedones and may be principally used in skin care routine for oily skin[22]. Another study by Charakida ,et al indicates 53% in sebum production and significant improvement in lesions assessed by Leeds acne grading system by using ethyl linoleate for 4 weeks [23]. Moreover, linoleic acid significantly decreases phagocytosis and reactive oxygen species generated by neutrophils [24]. Thus, a practical role for lipid dysregulation in acne pathogenesis and its correction stays a demanding area for research in treatment and regulation of squalene peroxidation generated by neutrophils gland hyperactivity.
Stimulatory effect of androgens on sebocytes has been well known in vitro and in vivo. However, various species of androgens function differently on sebcacous glands locationwise. Facial sebocytes are under influence of testosterone and dihydrotestosterone (DHT) with later having the strongest effect while body sebocytes are up regulated by dihydrotestosterone (DHT) and their proliferation affected negatively by testosterone [25]. Inhibitory effect of acylceramide with linoleic acid on keratinocytes hyperplasia induced by UVB exposure [26].
1. Harris HH, Downing DT, et al.
Sustainable rates of sebum secretion in acne patients and matched normal control subjects. J American Academy of Dermatology. 1983;8(2):200-203.
2. Cunliffe WU, Dunitz M. In: Acne. 1989.
3. Pierard-Franchimont C, Pierard GE, et al. Comparison of the kinetics of sebum secretion in young women with and without acne. Dermatologica. 1991;183(2):120-122.
4. Stewart ME, Grahek MW, Wertz WW, et al.
Dilutional effect of increased sebaceous gland activity on the poroportion of linoneic acid in sebaceous wax esters and in epidermal acylceramides. J Invest Dermatol. 1986;87(6):733-6.
5. Downing DT, Strauss JS, et al. Essential fatty acids and acne. J Am Acad Dermatol. 1986;14(2 Pt 1):221-5
6. Downing DT, Stewart ME. Meseaurement of sebum secretion rates in young children. J Invest Dermatol. 1985;84:59-61.
7. Stewart ME, Quinn MA, et al.
Variability in the fatty acid composition of wax esters from vernix caseosa and its possible relation to sebaceious gland activity. J Invest Dermatol. 1982;78:291-295.
8. Matoltsy AG. Keratinization. J Invest Dermatol. 1976;67:20-25.
9. Yamamoto A, Takenouchi K, Ito M. Impaired water barrier function in acne vulgaris. Arch Dermatol Res. 1995;287(2):214-8.
10. Schutze S, Pottoff K, Machleidt T, et al.
TNF activates NF-kappa B by phosphatidylcholine-specific phspholipase C-inuced acidic shingomyelin breakdown. Cell. 1992;71(5):765-76.
11. Summerly R, Yardley H J, Raymond M, et al. The lipid composition of sebaceous glands as a reflection of gland size. Brit J Dermatol. 1976;94(1):45-53.
12. Chiba K, Yoshizawa K, et al. Comdeogenicity of squalene monohydroperoxide in the skin after topical application. J Toxicol Sci. 2000;25(2):77-83.
13. Picardo M. Zompetta C, De Luca C, et al. Role of skin surface lipids in UV-induced epidermal cell changes. Arch Dermatol Res. 1991;283:191-197.
14. Zouboulis CC. Propionibacterium acnes and sebaceous lipogenesis: A love-hate relationship? J Invest Dermatol. 2009;129:2093-2096.
15. Miller CC, Tang W, Ziboh VA, Fletcher MP.
Dietrary supplementation with ethyl ester concertates of fish oil (n-3) and borage oil (n-6) polyunsatrated fatty acids induces epidermal generatio of local putative anti-inflammatory metabolites. J Invest Dermatol. 1991;86(1):98-103.
16 Strauss JS, Pochi PE, whitman EN. Suppression of sebaceous gland activity with Eicos-5:8:11:14-Tetraynoic acid. J Invest Dermatol. 1967;48(5):492-493.
17. Clarke BA, Clark DC.
Suppression of rat liver fatty acid synthesis by Eicosa-5,8,11,14-tetraynoic acid without a reduction in lipogenic
enzymes. J Nutr. 1982;112:1212-1219.
18. Zhao G, Etherton TD, Martin KR et al. Anti-inflammatory effects of polyunsaturated fatty acids in THP-1 cells. Biochem Biophys Res commun. 2005;113:1011-1020.
19. Zouboulis CC. Acne and sebaceous gland function. Clin Dermatol. 2004;22(5):360-6.
20. Liao S. Androgen action: molecular mechanism and medical application. J Formos Med Assoc. 1994;93(9):741-51.
21. Zouboulis CC, Seltmann H, Fritsch M, et al.
The human sebocyte culture model provides new insights into development and management of seborrhea and acne. Dermatology. 1998;196(1):21-31.
22. Detawe C, Boone M, Pierard GE.
Digital image analysis of effect of topically applied linoleic acid on acne microcomedones. Clin Exp Dermatol. 1998;23(2);56-8.
23. Charakida A. Chu AC, et al.
Double-blind, randomized, palcebo-controlled study of a lotion containing triethyl citrate and ethyl linoleate in the treatment of acne vulgaris. BR J Dermatol. 2010;163(2):437.
24. Akamatsu H, Komura J, Miyachi Y, et al. Suppressive effects of linoleic acid on neutrophil oxygen metabolism and phagocytosis. J invest Dermatol. 1990;95(3):271-4.
25. Akamatsu H, zoubooulis CC, Orfanos CE.
Control of human seobocyte proliferation in vitro by testosterone and 5-alpha-dihydrotestosterone is dependent on the localization of the sebaceous glands. J Invest Dermatol. 1992;99(4):509-511
26. Imokawa G, Yada Y, Kawamata A, et al.
Peudo-acylceramide with linoleic acid produces selective recovery of diminished cutaneous barrier function in essential fatty acid deficient rats and has an inhibitory effect on epidermal hyperplasia. J Clin Invest. 1994;94(1):89-96.
* Lovaszi. M, Sebaceous immunobiology is orchestrated by sebum lipids. Dermatoendocrinol, 2017 Oct 17;9(1)