There is no single best mode for management of all lesions . Acne treatment is determined by many factors, including the type of lesions present, duration of disease, past and present response to treatment, tendency for scarring and development of acne spots and more importantly severity of disease. Knowing the symptoms and treating acne lesions early and adequately are the keys to a successful management. Acne is a chronic disease and poor adherence to treatment is a major contributor to unresponsiveness [3].
Comorbidities and current use of medications especially oral contraceptives, corticosteroids and topical antibiotics may affect management . Psychological factors may have great impact on therapeutic plans [4]. Also adult patient’s overall hygiene, facial care, hair grooming, mechanical manipulation of lesions and use of cosmetics must be considered. There are two important points that acne patients should be aware of. First, six to eight weeks of acne treatment is required before improvement is noted [5]. Change of the regimen or addition of a new agent should be withheld during this period. Second, body lesions including back, chest, shoulder lesions respond more slowly to topical applications than do those on the face.
Some authors suggest addition of one agent, topical or systemic, at a time and implementation of the regimen for at least eight weeks before any change or addition of another agent could be made [5]. It is important to note that moderate to severe acne must be consulted with a physician in particularly to diagnose variants of acne vulgaris of more severe cystic form such as acne conglobata with more weighty psychosomatic impact.
According to guidelines, acne management would be based on severity of acne lesions. Mild, moderate and severe acne are to be treated with different management protocols. Mild form (grade I) is treated with topical retinoid with or without benzoyl peroxide. Topical clindamycin or erythromycin could be added if no adequate response withing eight weeks. For moderate acne (grade II-III) oral antibiotics can be started.
Hormone therapy, oral contraceptive or progesterone preparations, for females are added in more severe forms. Warranting systemic modalities, cysts treatment is either isotretinoin or combination of what is indicated for mild to moderate forms. Here you can find more information on maintenance treatment and its algorithm based on acne grade. Evidently, isotretinoin and antibiotic therapy is not included in acne maintenance treatment, which targets comedogenesis, for their potential side effects and toxicity. Maintenance treatment is necessary to prevent development of microcomedones.
Acne skin care, commonly overlooked by physicians, may work by itself in mild to moderate acne without implementing any pharmacological regimen. Among the benefits of any non-pharmacologic regimen, less antibiotic resistance, a more nature-conscious choice, much less side effects including contact dermatitis and skin irritations could be counted. Change in composition of sebum, type of fatty acids, squalene increase and skin’s mantle call for a skin care which respects this alteration and address this frequently-discounted fragment of acne pathology [10]. Alteration in skin’s microbiome and the equilibrium between the two main skin’s commensals, C. acnes and S. epidermidis, has been purported to breed inflammation by modifying skin surface’s lipids and its manipulation hold sufficient promise to deserve an opportunity in treatment armamentarium of acne vulgaris.
On the other hand, burgeoning evidence hypothesizes that the microbiome dysbiosis may be modulated by non-microbial factors such as diet, hormones or skin type. Achievements of nutriceutical interventions aimed at restoring normal skin surface lipid composition and homeostasis are feasible therapeutic goals [11] [12]. Multitude of studies suggest a direct relationship between high glycemic index foods and acne vulgaris, demonstrating diets devoid of western refined foods ameliorate non-inflammatory and inflammatory acne.
In parallel to these studies, dairy have been found to be acneogenic due to their insulinotropic effects by enhancing IGF-1 or insulin itself. On the other hand, randomized controlled studies cast doubt on precedent works which gainsaid any association between diet and dietary habits with acne severity by revealing an increase in level of anti inflammatory fatty acids with consumption of mixed probiotics.

In contrast to antibiotics, resident organisms do not become resistant to this agent. This anti acne agent also demonstrates mild anti-inflammatory activity [14]. Its comedolytic property is comparatively slight in contrast to other topical agents used for treatment of acne. Benzoyl peroxide reduces sebum secretion by 22.5%.after 2 months use [15]. Contact allergy is quite rare with it. Skin irritation is considerable. Synergistic effect this agent has been shown with antibiotics such as erythromycin and clindamycin in topical preparations [16] [17]. On the other hand, cytotoxicity and reactive oxygen species, ROS, associated with use of this modality warrants concurrent utilization of antioxidants in any evidence based skin care regimen which targets bacterial colonization axis as primary culprit in acne vulgaris.
Among comedolytic treatment agents salicylic acid [18], which could be used as alternative or adjunct to benzoyl peroxide, is considerably being used. This combination therapy has been associated with favorable outcomes among modalities for moderate acne forms. Salicylic acid comedolytic activity justifies its therapeutic value in acne. Keratolytic activity of this BHA causes peeling and removal of top layer of the skin. This can result in preventing the follicles from getting plugged. Salicylic acid is also moderately potent in destructing Porpionibacterium acnes and shows moderate antibacterial efficacy.
pH control is another means to treat acne as proprionibacterium acne alters skin’s pH and its modification may have a role in acne treatment. Application of alpha hydroxy acids may resolve the comedones and prevent more severe acne such as cysts. Use of hydroxy acids,AHA’s, alone is not indicated for acne. However, a positive effect through control of sebum production and ductal hypercornification is likely. Peels of alpha and beta hydroxy acids have been shown of efficacy in control of oily skin [19]. Azelaic acid in 10-20% preparation have been used with promising results, however, some studies have been found benzoyl peroxide superior to azelaic acid in treatment for acne vulgaris. Topical azelaic acid was also found effective to control rosacea by barring ROS production and quenching inflammation.
Antioxidants are another category amid long term goals for acne therapy. Superoxide and other free radicals production appear to be involved in aggravation of acne vulgaris. Proprionibacterium acne may be accounted for superoxide’s radicals generation. Among antioxidants alpha lipoic acid, bioflavanoids and sea buckthorn have been subject of some studies and suggested by them in management. Oxidative stress exists in patients with acne vulgaris and play a role in etiopathogenesis and/or progression of the disease. The addition of modalities with antioxidative effects seems to be valuable in the control of acne vulgaris [20]. Certain antioxidants are well- known for their inhibitory effect on androgens. Genistein is non-steroidal inhibitor of 3-beta-hydroxysteriod dehyrodrogenase, zinc, gamma-linolenic, alizarin and curcumin are non-steroidal inhibitors of 5-alpha-reductase [21].
Sodium ascorbyl phosphate lotion demonstrated statistically significant improvement when compared to vehicle in all of the parameters measured. The adverse event frequency and cutaneous tolerability profile for sodium ascorbyl phosphate lotion were similar to vehicle [22]. Mangensium ascorbyl phosphate serum has also been associated with favorable outcomes in patients with acne through perpetual delivery of vitamin C and its inhibitory impact on lipid peroxidation.
Lauric acid one of the typical fatty acids found in the human sebum, shows stronger antimicrobial activity than benzoyl peroxide while not inducing any cytotoxicity to human sebocytes [24]. However of drawback of lauric acid is its poor water solubility. It requires a solvent such as dimethylsulfoxide (DMSO), which is very irritant to the skin. Incorporation of lauric acid in liposomal form, whichh enhances its absorption, has eliminated us of DMSO [23].
Another category of topical treatments are plant based extracts and oils, namely, Leptospermum scoparium or manuka oil, from the tea tree family yet still a distinct plant with more robust antimicrobial properties. Its main constituents are leptospermone, calamenene, falvesone, cadine-3,5-diene and α-copaene with wide bactericidal and bacteriostatic effects on a range of gram positive, more prominent effect, and gram negative bacteria and fungi, among them, C. acnes (MIC=0.211 and 0.055 reported by two different studies) and S. epidermidis (MIC=1.40) whose dysbiosis recognized in pathogenesis of acne vulgaris.
Cell lysis of staphylococcus aureus with concentration of manuka oil as low as 1.5% have been shown with β-triketone known as the accountable constituent. Other plant oils with antibacterial effect on C. acnes have been studied and reported, thyme with MIC=0.016, cinnamon with MIC=0.016, and rose with MIC=0.016 are among the most notables. Certain amalgamations of essential oils demonstrated synergism and vigor to pulverize pathological microorganisms with propitious safety profiles and encouraging applicability to attenuate acne.
Marine extracts from kelp and algae have been novel focus of several studies for their polemic antimicrobial properties, albeit their bioactives against C. acnes and S. epidermidis appears as provably substantial avail. Among the plethora, fucofureckol-A from the kelp Eisenia bicyclis was found to be most remarkable with MIC of 32-128 μg/ml and in combination with erythromycin significantly reduced to 1μg/ml. On the other hand, glycolipids of marine algae, as cardinal element, were demonstrated with antioxidant and antimicrobial traits with two major biogenic groups of neutral galactolipids and sulfolipids. Galactolipids of brown algae Fucus evanescens was discovered accountable for inhibitory efficiency against C. acnes with MIC of 50μg/ml with montogalactosyldiacylglycerol as effectual compound.
Topical timolol has been subject of some late studies in an effort to broaden the acne treatment armamentarium for its vasoconstricive, antiangiogenic and anti inflammatory effect while precedent research did not add up to a supportive pattern for propronolol. Timolol, a not selective β-blocker demonstrates inhibitory impact on matrix mataloproteinases, MMP-2, MMP-9 and IL-6 while carrying a more favorable safety profile. A study of 114 patients of acne vulgaris and rosacea with no control cohort for eight weeks has shown efficacy of timolol in control of acne and rosacea, largely, due to its reach in thwarting inflammation and vasoconstriction-led decrease in sebum production.
Tretinoin is another topical modality that could be used to treat acne vulgaris. This derivative of Vitamin A is keratolytic and may cause a form of dermatitis called retinoid dermatitis. It could be combined with antibiotic to address other etiologies involved in formation of acne lesions. One of these combinations is tretinoin-clindamycin that one study indicates its increased efficacy. Another retinoid combination is with benzoyl peroxide that one study suggests its efficacy [25]. New retinoids(adapalene) have shown to have anti-inflammatory effects which aims to another mechanism in development of acne, inflammation (increase in IL-1 and TNF). This reserves use of retinoids in management of inflammatory lesions as well as previously-explained non inflammatory acne.
Isotretinoin is among oral medications used in severe cases of acne through concurrent reduction in hyperkeratinization and associated inflammation [26]. Isotretinoin has a profound impact on sebaceous gland size and function, thereby decreasing serum level of more active androgens [27]. The marked sebostatic effect of isotretinoin may not be be the sole explanation for its mechanism of action [28]. Retin-A tretinoin (topical form of isotretinoin) is among acne modalities to get rid of breakouts especially when other forms of therapy has failed. Tretinoin is a prescribed drug and an skin irritant particularly in liquid form with extensive adverse effect profile. Cold climates and exposure to sunlight cause marked irritation. Retin-A (tretinoin) precipitates antikeratinization and prevents formation of the comedones.
Among topical retinoids, adapalene, a more receptor-selective retinoid, shows the best tolerability/safety profile followed by isotretinoin and tretinoin [29]. Retin-A differs from benzoyl peroxide and topical antibiotics in having no or a controversial effect on Porpionibacterium.acnes and causing no direct effect in surface free fatty acids. Tretinoin seems compelling against microcomedones (a blackhead) compare with other treatment modalities provides a rationale for its use in most forms of acne. This agent is particularly helpful in reducing non-inflamed lesions and comedones thereby indirectly reduces the number of inflamed blemishes by correcting the follicular hyperkeratosis.
This drug is a powerful exfoliant and can cause tenderness, redness and scaling. Antibiotics may be used in moderate to severe cases of acne. Tetracyclin, Erythromycin and Clindamycin are more commonly used. Their potential side effects and development of resistance discourage their use for long term and renders them not a proper choice in acne maintenance therapy [30]. Use of medicinal plants and herbal preparation have been widely exercised in topical treatments or in and oily skin care no significant avail as in most cases outcomes not measured and treatments not standardized.
Hormonal acne treatment affects the androgen-metabolizing cells of pilosebaceous unit, i. e. follicular kertinocytes and sebocytes, with a reduction of the sebum secretion rate of 12.5 to 65% [31]. Prescription of hormonal antiandrogen acne medications is limited to female patients who present additional signs of peripheral hyperandrogenism or hyperandrogenemia. In addition, females with acne tarda, persistent acne recalcitrant to treatment, parallel with contraception as a requirement for a systemic isotretinoin treatment, can be treated with hormonal antiandrogens [31].
Topical and systemic antibiotics have been the mainstay of acne management protocol for over 50 years. Incidence of antibiotic resistance in acne has continued to rise across the globe from 20% in 1978 to 72.5% in 1995 [32]. Antibiotic resistance in acne represents a significant international public health concern because resistance can occur in more pathogenic bacteria than P. acnes, and an increase in pathogenic P. acnes has been reported [33]. Emerging antibiotics resistance of P. acnes is a ground for attention and a reminder of a need to modify the current acne guidelines [34]. Furthermore acne vulgaris is not primarily a bacterial infection and other pathological factors, if not more significant, appear to be equally substantial. Thus, treatment with modalities which address pathologies other than bacterial side of acne pathology are more gravely called for.
Products that may cause irritation are widely used for control of acne with the potential to reduce treatment adherence [35]. Topical retinoids often cause severe local irritation called retinoid dermatitis [36]. Cytotoxicity associated with tretinoin and benzoyl peroxide [37] demand a new therapeutic approach, in particular a different regimen as maintenance treatment. New modalities with safer side effect profile seem to be more promising in maintenance and may require incorporation into therapeutic guidelines.
It is of note that global grading system and lesion (papule, pustule, comedone) counts are equally reproducible methods of grading inflammatory acne which significantly contributes to follow up of any regimen to control comedones[38].
Mild form: Comedones, whiteheads and blackheads, few papules or pustules seen. An open comedone is defined as a non-inflamed follicular opening containing a keratotic plug that appear black, a blackhead [39]. The closed comedone, whitehead, contains less compact keratinous material and has a narrow follicular orifice [40]. Topical agents are indicated only. Benzoyl peroxide, topical clindamycin, topical erythromycin, or a combination [41] could be used.
Moderate acne: Papules and pustules frequently seen, One nodule may be occasionally found. Topical as well as systemic agents, if no response withing eight weeks, may be started. Topical tretinoin or adapalene, systemic tetracyclin are most frequently used.
Severe: Nodules and cysts commonly found. Even presence of a few of these type categorized as severe. Presence of cysts requires treatment with systemic agents such as isotretinoin (first line) or anti-androgenic agents even though some more recent studies suggest a trial of topical treatments as initial approach has been associated with more frequent treatment failures. Scarring can be counted as severe acne.
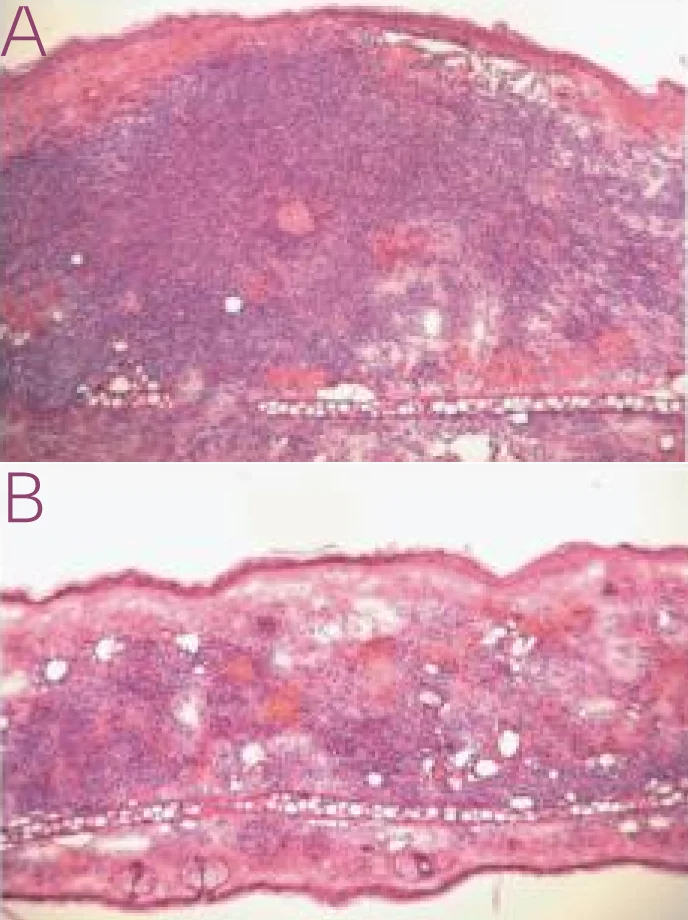
Effect of lauric acid against Propionicbacterium. acnes has been demonstrated. See resolution of inflammation on the right after injection of lauric acid into the skin. On the left the skin is not treated with lauric acid [24].
1. Burkhart C, Gottwald L. Assessment of etiologic agents in acne pathogenesis. Skinmed. 2003;2(4):222-8.
2. Thiboutot D, Harness J, Janiczek-Dolphin N, et at. Can sebum reduction predict acne outcome?Br J Dermatol 2010; 163:683-88.
3. Yentzer BA, Ade RA, Fountain JM, et al. Simplifying regimens promotes greater adherence and outcomes with topical acne medications: a randomized controlled trial. Cutis 86(2):103–8 (2010 Aug).
4. Kimball, AB, Chon SY. Response of skin disease to stress: changes in the severity of acne vulgaris as affected by stress. Arch Dermatol. 2003;139(7):897-900
5. Tallia A, Scherger J, Dickey N. Swanson family medicine review (2009), 6th edition.
6. Thiboutot, D., & Gollnick, H. (2009). New insights into the management of acne: An update from the Global Alliance to Improve Outcomes in Acne Group. Journal of the American Academy of Dermatology, 60, S1–S50.
7. Youn SW, Park ES, Lee DH et al. Does facial sebum excretion really affect the development of acne? Br J Dermatol 2005; 153:919–24.
8. van Vloten WA, van Haselen CW, van Zuuren EJ et al.The effect of 2 combined oral contraceptives containing either drospirenone or cyproterone acetate on acne and seborrhea. Cutis 2002; 69:2–15.
9. Zouboulis CC, Nestoris S, Adler YD et al. A new concept for acne therapy: a pilot study with Zileuton, an oral 5-lipoxygenase inhibitor. Arch Dermatol 2003; 139:668–70.
10. Saint-Leger D, Baque A, Cohen E, Lchivot M. A possible role of squalene in the pathogenesis of acne. In vitro study of squalene oxidation. Brit J Dermatol. 1986;114(5):535-542.
11. Logan AC, Cordain L. Omega-3 fatty acids and acne. Arch Dermatol 2003;139(7):941-943
12. De Luca C, Valachi G. Surface lipid as multifunctional mediators of skin responses to environmental stimuli. Mediators Inflamm. 2010;2010:321494.
13. Fulton JE Jr. Studies on the mechanism of action to topical benzoyl peroxide and vitamin A in acne vulgaris. J Cutan Pathol 1974;1(5):191-200.
14. Burkhart CK. A re-examination of the function of benzoyl peroxide in acne. J Dermatol Allergy 5:23-6 (1982).
15. Cunliffe WJ, Stainton C, Forster RA. Topical benzoyl peroxide increase the sebum excretion rate of pationts with acne. Br J Dermatol 109(5):577-9 (1983).
16. Eady EA, Bojar RA, Holland KT, Culiffe Wj. The effect of treatment with a combination of benzoyl peroxide and erythromycin on skin carriage of erythromycin resistant propionibacteria. Br J Dermatol 134(1):107-13 (1996).
17. Lookingbill DP, et al. Treatment of acne with a combination clindamycin/benzoyl peroxide gel. J Am Acad Dermatol 37(4):590-5 (1997).
18. Pham M, Efficacy and tolerability of a combination of benzoyl peroxide, salicylic acid for treatment of adult acne. J Am Acad Dermatol. 2009; 60(3):AB21
19. Kessler E, et al. Comparison of alpha and beta hydroxy acid chemical peels in treatment of mild to moderate acne vulgaris. Dermatologic surgery 2008; 34:(1);45-51.
20. Nermeen S.A. Tissue and blood superoxide dismutase activities in different clinical severities of acne vulgaris. Brit J Dermatol. 2008;159(5):1086-91.
21. Chen, WC, Thiboutot D, Zouboulis CC. Cutaneous androgen metablolism: Basic research and clinical perspectives. J Invest Dermatol. 2002;119:992-1007.
22. Woolery-Lloyd H. Baumann L, Ikeno H. Sodium L-ascorbyl-2-phosphate 5% lotion for the treatment of acne vulgaris: a randomized, double-blind, controlled trial. J Cosmet Dermatol. 2010;9(1):22-7.
23. Yang D, Carson D, Zhang Liangfang, et al. The antimicrobial activity of liposomal lauric acid against propionibacterium acnes. Biomaterials. 2009;30(30):6035-40.
24. Nakatsuji T, Kao MC, Fang JY, Zouboulis CC, Zhang L, Gallo RL. Antimicrobial property of lauric acid again P. acnes: Its therapeutic potential for inflammatory acne vulgaris. J Invest Dermatol. 2009;129(10):2480-8.
25. Hughes BR, Norris JFB, Cunliffe WJ. A double-blind evaluation of topical tretinoin 0.05%, benzoyl peroxide gel 5% and placebo in patients with acne. Clin Exp Dermatol 1992; 17:165–8.
26. Hughes BR, Cunliffe WJ. A prospective study of the effect of isotretinoin in the follicular reservoir and sustainable sebum excretion rate in patients with acne. Arch Dermatol 1994; 130:315–18.
27. Lookinngbill D, Demers L, et al. Effect of isotretinoin on serum levvels of precursor and peripherally derived androgens in acne. Arch Dermatol. 1988;124(4):540-543.
28. Goldstein J, Comite H, Mescon H. Isotretinoin in treatment of acne, histologic changes, sebum production and clinical observations. Arch Dermatol. 1982;118(8):555-558.
29. Degitz R Erdmann, et al. European evidence-based guidelines for treatment of acne. J Euro Academy Dermatol. 2012, 26(1):1-29.
30. Ross JI, Snelling AM, Carnegie E, et al. Antibiotic resistant acne: lessons from Europe. Br J Dermatol. 2003;148(3):467-78.
31. Zouboulis CC, Rabe T. Hormonal antiandrogens in acne treatment. J Dtsch Dermatol Ges. 2010;Suppl 1:S60-74.
32. Cooper AJ. Systematic review of P. acnes resistance to systemic antibiotics. Med J Aust. 1998;169(5):259-61.
33. Humphrey S. Antibiotic resistance in acne vulgaris. Skin Therapy Lett. 2012;15(86):734-40.
34. Mobacken H, Oprica C, Berg M. New treatment strategy in acne vulgaris. Antibiotic prescription must be limited. Lakartidningen. 2012;109(22):1085-9.
35. Feldman SR, Chen DM. How patients experience and manage dryness and irritation from treatment modalities for acne. J Drugs Dermatol. 2011;10(6):605-8.
36. Kim B, Lee JD, et al. Co-treatment with retinyl retionate and a PPAR-alpha agonist reduces retinoid dermatitis. Int J Dermatol. 2012;51(6):733-41.
37. Bulinckx A, Dachelet C, Leroy A, Goossens A, Tennstedt D, Baeck M. Contact dermatitis to the combination gel of adaplene 0.1% and benzoyl peroxide 2.5%. Eur J Dermatol. 2012;22(1)139-40.
38. Bruce Allen, Graham Smith. Various parameters for grading acne vulgaris. Arch Dermatol 1982, 118(1): 23-25.
39. Feldman S, Careccia RE, Braham KL, Hancox J: Diagnosis and treatment of acne. Am Fam Phy 69:2123-2130, 2004
40. Burkhart CG, Burkhart CN, Lehmann PL. Acne a review of immunologic and microbiologic factors. Postgrad Med J. 1999ert;75:328-331.
41. Jones T, Monroe E, Weiss J. A multicenter study to evaluate erythromycin Benzoyl Peroxide Dual-Pouch Pack for Acne vulgaris. Clin Drug Invest. 2002;22(7).