
Most affected sites are face, back, shoulder and chest in form of papules, nodules, cysts, pustules as well as comedones which are frequently experienced without inflammatory component. It may lead to acne conglobata, a more severe presentation, adamantly inflammatory, with cysts interconnected abscesses, or acne fulminans, with systemic manifestations such as fever and arthritis. In the same spectrum of skin disorders with distinct pathogenesis is acne rosacea whose treatment approach , vary greatly from that of vulgaris type of acne. With early diagnosis and prompt, appropriate treatment, acne lesions may be kept under control and complications such as scars avoided.
In most cases the manifestations of acne are worse in winter and improves during the summer, suggesting a beneficent effect of sunlight, which might be due to its effect in enhancing vitamin D. However, in some cases exposure to sunlight worsens the disease. The constant friction caused by protective devices such as a helmet, shoulder pads or pillows will make its management more difficult simultaneous with higher likelihood of skin scarring. Rupture of sebaceous follicles (a cutaneous gland that secretes sebum) is among other aggravating factors. Rupture could be result of skin injury by mechanical squeezing of lesions, abrasive scrubbing of the skin or skin resurfacing methods such as dermabrasion.
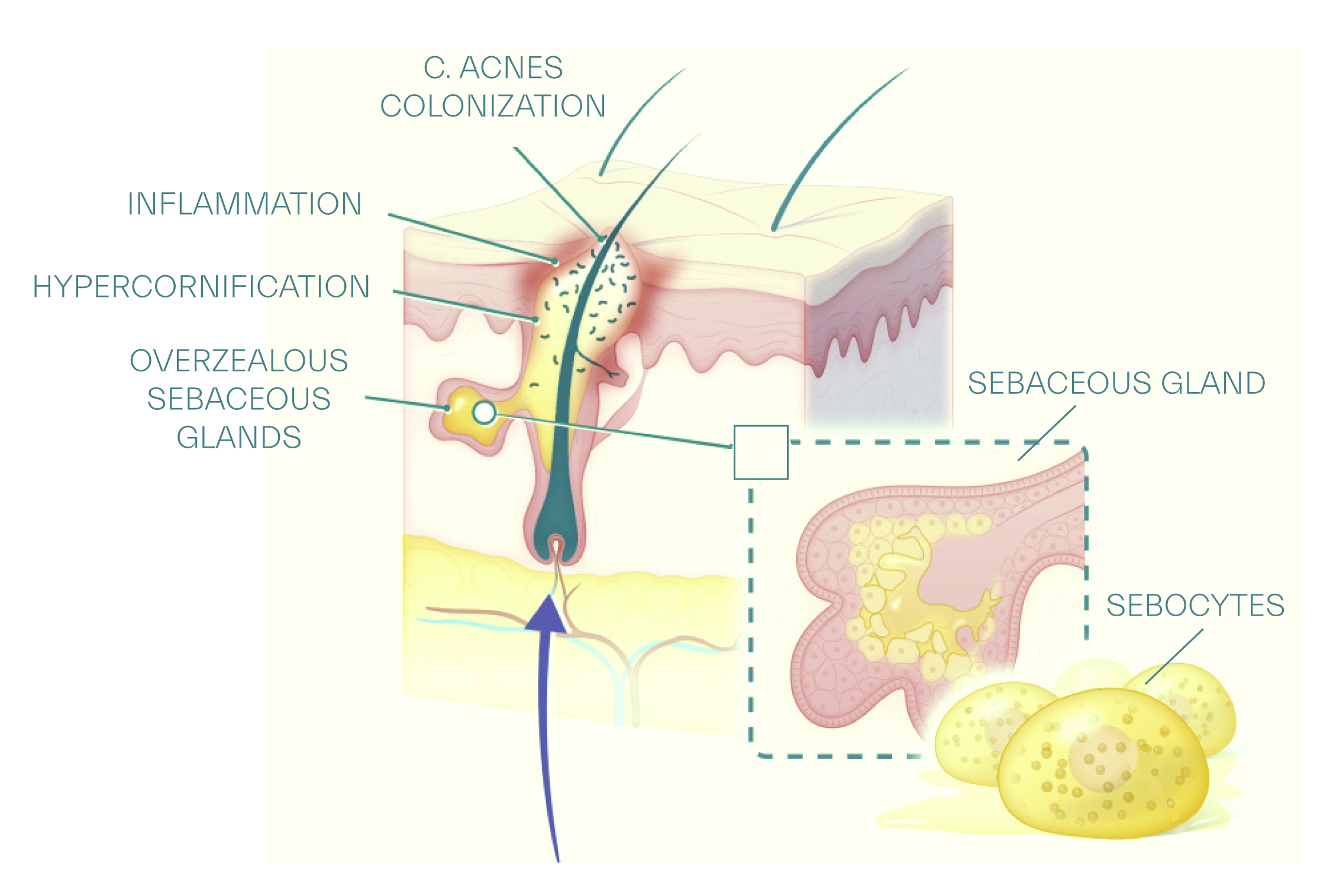
Comedones, commonly termed, whiteheads, closed comedones and blackheads, open comedones are considered inflammatory in most recent nomenclature as presence of inflammation has been found even before hyperproliferative stage of sebaceous follicle at microcomedo level. Other inflammatory lesions are papules, nodules and cysts. Areas of the body where hair follicles are of highest population as in face, shoulders, back, chest and upper arms most frequently affected.
Comedones:
No papule or nodule seen in this stage, closed or open comedones are present. A comedo is a blocked pore, which leads to a sebaceous gland. It may be black in appearance due to its oxidized sebum as in open comedones, or skin color with a slight inflammation in closed comedones.
Papules:
Papules are red lesions, colloquially known as pimples, small, less than 1 cm, red, circumscribed, elevated and superficial, largely epidermal involvement.
Pustules:
Pustules are similar to papules but with a central collection of white pus at their top. Pustules look yellow with a pus component on top, a superficial elevation and circumscribed, in greater number and in a wider area
Nodules:
Nodules are tender and feel hard on palpation, larger than 5 mm in size, with dermal and subcutaneous involvement. Nodules are deep-seated structures and tend to remain for as long as eight weeks before finally resolving.
Cysts:
Cysts are fluctuant nodules containing fluid. Cysts are not very common types, a common manifestation of stress, but when they occur they may reach several centimeter in diameter. Cysts are tender, sensitive, deeper and larger pimples filled with pus. Cystic form is considered among severe acne types and its treatment must be consulted with a physician. Cystic acne cure may take longer period of time and its recurrency is very likely.
Severity, extent and size of lesions, and not inflammation may be employed in staging and diagnosis of acne vulgaris as all lesions including comedones classified as inflammatory. Four stages which pragmatically influence management and treatment protocols are as the following:
Comedonal acne: no papule or nodule seen in this stage, closed or open comedones are present, a comedo is a blocked pore which may appear black, oxidized sebum as in open comedones, or appear skin color with a slight inflammation in closed comedones
Mild acne: a few papules, small, less than 1 cm, red, circumscribed, elevated and superficial, mostly epidermal involvement. A mixture of comedones and papules is also considered a mild form.
Moderate acne: papules, pustules, look yellow with a pus component on top, superficial elevation and circumscribed, in greater number and in a wider area, mild scarring is seen.
Severe acne: nodules and cysts are seen in addition to papules and pustules. Nodules are tender and feel hard on palpation, larger than 5 mm in size, with dermal and subcutaneous involvement and cysts are fluctuant nodules containing fluid. Scarring apt to more prominent.
Acne vulgaris mangement is aimed at addressing the etiological factors known in its pathogenesis. Thus, sebum regulation, control of inflammation, obliteration of acne bacteria and combating hyperkeratinization are mainstay of acne treatment approach which primarily engages in reconciliation with its etiopathogenesis. Therapy for acne with multiple agents is associated with more favorable outcomes as some of the agents has been conceived having synergistic effects
Treatment of exacerbations
Comedonal acne: topical retinoids, resistant cases are treated similar to mild acne
Mild acne: retionoids plus benzoyl peroxide
Moderate acne: retioids plus benzoyl peroxide plus topical antibiotics (erythromycin, clindamycin), oral antibiotics used for treatment of nodules
Severe acne: oral isotretionin
Resistant cases of each stages are treated akin to that of one stage higher
Maintenance treatment
Recognized as a chronic disease, maintenance treatment is fundamental to treatment of acne and starts when an exacerbation subsides.
Comdeones: topical retinoids
Mild acne: topical retinoids
Moderate acne: topical retinoids plus benzoyl peroxide
Severe acne: topical retinoids plus benzoyl peroxide plus topical antibiotics
Topical treatments, prescription
Topical retionoids counteract follicular hyperkeratinization by which reduce number of comedones, normalize desquamation and prevent formation of new comedo while they possess anti inflammatory properties by suppression of toll-like receptors and blocking release of cytokine and nitric oxide, inhibiting cellular inflammation.
Topical antibiotics are mainly used to treat mild to moderate forms and used in combination with benzoyl peroxide to prevent resistance formation. Erythromycin and clindamycin are most widely-studied antibiotics tried in acne management. Concept of combination therapy robustly substantiate clinical efficacy in treatment of inflammatory acne and is settled as standard of care in management of moderate to severe acne by multitude of studies, amid them one randomized double blind controlled study advocates superiority of combination of adapelene with benzoyl peroxide compare to vehicle.
Topical treatments, over the counter
Benzyol peroxide has been extensively researched and utilized in treatment of mild to moderate acne exacerbations as well as maintenance treatment of severe acne. It appears idiosyncratic among most well-known acne modalities, in that it does not invoke bacterial resistance. No concentration of this agent seem to be superior to others, however, superiority of various pH and their compatibility with skin’s mantle pH has not been studied. Generating reactive oxygen species, benzoyl peroxide destruct bacterial proteins and demonstrates bactericidal effects. Frequently reported as skin irritant, this agent causes contact dermatitis in particular in those with atopic dermatitis.
Salicylic acid,a beta hydroxy acid, is widely used over the counter topical treatment with keratolytic and comedolytic effects. Impact of salicylic acid on skin cells is elicited through breakage of intercellular desmosomes, enhancing corneocytes desquamation. Some studies suggest dermal proliferation and increase in dermal glycosaminoglycosides with use of hydroxy acids comparable to that of topical retionids.
Concept of evidence-based acne skin care is growing in medical literature and and its use becomes more compelling as an adjunctive or non-adjunctive treatment in management of acne vulgaris for multitude of rationals. Utilization of several evidence-based ingredients in an skin care which is more genial to the skin in terms of respecting pH of skin and provision of skin essential nutrients and integral moisture-sustaining proteins seems to be more promising as opposed to various formulations which change the composition of skin surface lipids and deprive the skin of its proteins.
Skin cleansers, face washes containing alcohol, various soaps tend to create an alkaline skin pH, droughty epidermis which precipitates sebaceous glands to increase their secretions to overcome drenched, lipid depleted skin. The scenario is even more exaggerated in acne patients using oil-free skin products by giving rise to overzealous sebaceous glands, compelled to excrete more sebum, to bargain the counterbalance neutralized. The composition of sebum in overly-stimulated sebaceous units is gravely affected by turning on a mode to form less virtuous fatty acids, less salubrious skin mantle inflicted by imbalance of its essential fatty acids, a change in ratio of unsaturated fatty acids to saturated fatty acids, associated with comedogenesis.
Non hormonal Oral treatments
Oral antibiotics are primarily used in moderate to severe forms of acne for a period of exacerbation and can be discontinued upon remission while maintenance treatment started to prevent relapses. Some authors propose limiting antibiotic use to three months or less and in combination with non-antibiotic treatments. Use of adjunctive benzoyl peroxide has been suggested to prevent bacterial resistance. Tetracycline, minocycline, erythromycin, clindamycin and trimethoprime/sulfamethaxazole are among the most frequently prescribed oral antibiotics for acne treatment. Doxycycline and minocylcine are preferred over tetracycline, which is associated with lower rate of bacterial resistance compare to that of erythromycin.
Isotretinoin used in severe recalcitrant acne affects almost all aspects of acne etiology by reducing follicular keratinization, tempering excess sebum production, combating bacterial activity and inflammation. Isotrentinoin is notorious for a quite broad range of adverse effects which may affect treatment adherence. Hypertriglyceridimia, pancreatitis, teratogenicity, increased susceptibility to autoimmune disease namely celiac disease, blood dyscrasias, Steven-Johnson syndrome, toxic epidermal necrolysis and psychiatric illness, depression, psychosis, anxiety are amid most well studied side effects. Twenty percent of isotretinoin treated patients have a relapse which require retreatment with this agent while forty percent can be treated with other modalities used in treatment of mild to severe acne.
Hormonal oral treatments
Acne is understood as hormonally mediated disease with cutaneous hyperandrogenism induced by hyperfunction of sebaceous glands despite normal serum androgen levels. However, in certain cases, role of hormones becomes more prominent and consideration of hormonal acne treatment is warranted.
Oral contraceptives for treatment of acne containing combined estrogen, progesterone are considered fist line treatment especially in women with menstrual cycle associated flares or in treatment of acne associated with polycystic ovary syndrome or in adrenal hyperplasia associated with acne and hirsutism.
Spironolactone, an androgen receptor blocker, efficacy in treatment of acne vulgaris has shown equivocal results and its use in selective subpopulation of patients such as those with evidence of hormonal imbalance has not been determined and calls for further studies.
Non pharmocological treatments
Emerging studies in epidemiology of acne vulgaris cast doubt on precedent views on equivocal impact of diet in pathogenesis of acne vulgaris and portend a more transparent stance, indicative of direct association between certain diets and dietary factors with acne. Vitamin D, known for its comedolytic activity and regulatory role in proliferation and differentiation of sebocytes and keratinocytes, has been suggested to be deficient in clinically-evident acne patients. Lower expression of inflammatory markers, IL-6, IL-8, MMP-9 and inhibition of P.acnes induced IL-17 has been associated with vitmain D application. Another aspect of this narrative is the salutary effect of oral probiotics and gut microbiome on chronic perifollucular inflammation existent in early acne lesions, microcomedones. Omega 3 fatty acids have been subject of great enthusiasm to determine validity and clinical efficacy of their use in acne patients and gained rather solid ground in randomized controlled trials, showing improved outcomes.
As mere concern of bacterial resistance arises, more recent studies have been directed toward one significant novel focus, that is, seeking agents with neutrality or lack of this resistance. Exogenous utilization of long chained poly unsatruated fatty acids, LC-PUFA, have been subject of this attention for their known antimicrobial activity as seminal component of innate immune system against skin pathogens, p.acnes and staphyloccocus aureus. LC-PUFA synergy with skin antimicorbial peptides and with other modalities, benzoyl peroxide, concurrent with their provable beneficence in reducing use of antibiotics appeals to broader research work to find out their clinical pragmatism.
Low glycemic diets have been shown to reduce level of IGF-1, which leads to androgen-mediated increase in sebum production, a mechanism which meaningfully translate into clinical significance of diet in acne vulgaris patients. The nuanced view proclaiming acne vulgaris as mTORC-1 induced insulin resistance and metabolic syndrome does not seem to be on untenable grounds. Taken collectively, these findings provision burgeoning body of evidence on implication of dietary factors in pathogenesis of acne and create a paradigm for further studies which guide future management of this chronic disease. In this escalating anticipation a new cross-sectional study was initiated with aim to elucidate role of metabolic biomarkers, inflammatory markers, diet, sleep and stress level and their association with severity of acne.
Procedures:
Office peels such as glycolic acid peels, salicylic acid peels have succeeded with better outcomes compare to that of laser and light therapies in treatment of acne vulgaris, however, robust evidence for use of these modalities is lacking and more well-designed RCTs are called for to identify optimal regimens.
A Cochrane systematic review of 71 randomized control trials including 4211 participants found inefficacy of light therapy, photodynamic therapy, PDT, infrared light, blue light, yellow light and pulse dye laser in treatment of vulgaris type of acne. Another systematic review of 33 studies found circumstantial evidence for nonpharmocolgical treatment approaches which included light therapy, laser treatments and chemical peels to acne patients. These reviews on efficacy of laser procedures and light therapy demonstrate conflicting results and spawn uncertainty and controversy. These office procedures for acne treatment have not been generally included in guidelines as yet.
Intralesional steroid injection may be viewed with skepticism not for lack of effect but for its extensive adverse effects, even when used short term, including deleterious impact on skin barrier function and stratum corneum integrity even and the fact that this procedure can not be repeated for long time.